Robots and intelligent systems are revolutionising medicine
The impacts of artificial intelligence
- Dossier
- Jul 23
- 14 mins

Artificial intelligence (AI) is revolutionising medicine and healthcare. There are already developments that can identify tumours more accurately than human experts. A complex surgery such as an aortic valve implantation is hard to understand today without robotic systems supporting physicians. And thanks to data and algorithms, the road to personalised medicine is opening up.
Since its inception, AI has supported medicine and healthcare. As early as 1972, there was already an intelligent tool that could identify the bacteria causing a blood infection[1]. These early tools were called expert systems, because they sought to replicate the knowledge of a human expert in a field of application – medicine, in this case – with the aim of making this expertise accessible to a wide audience, e.g. hospitals lacking a certain type of specialist. However, the clinical practice of medicine is the use of the best available scientific evidence, usually by means of clinical trials, whose results are published in scientific articles. This is known as evidence-based medicine. In this regard, the knowledge of a system must be constantly reviewed, and the systems that support decision making – now known as clinical decision support systems – have become more complex.
Indeed, the clinical milieu has changed significantly since the first expert systems, and clinical information methods now collect a wealth of patient health care records, as well as genetic information and information obtained through new devices, including wearables.[2]. Data availability has allowed this medical evidence to be obtained not only through prospective clinical trials, which involves testing individuals, but also testing hypotheses using retrospective trials and information stored in our health systems. In addition, machine-learning methods are applied to data from health records to identify, for example, which individuals are at high risk of cardiovascular disease. With this information, physicians can recommend actions to prevent possible health deterioration.
In addition, genetic data brings us closer to what is known as precision medicine, which allows us to design specific drugs for patients with special health conditions, in accordance with their genetics. In fact, the generation of new proteins that allow the synthesis of new drugs is one of the focal points of the use of AI, which mainly uses techniques known as deep learning.[3].
As far as new devices are concerned, nowadays we have complex monitoring systems, medical imaging, assisted robotics… If we picture an ICU, we will see patients connected to many devices that monitor their vital signs. This amount of information is difficult to control for the person in charge of the patient, who is helped in the process by AI systems, activating alerts if risk situations are detected. These monitoring systems are developed on the basis of the case histories of patients who have experienced similar scenarios, some of whom have recovered while others, sadly, have not. For instance, there are systems that allow early detection of sepsis, a serious medical condition that can rapidly lead to death[4].
AI helps to identify critical episodes in patients with chronic illnesses and makes recommendations to prevent them from recurring.
In terms of wearables, new ways of collecting objective data for monitoring those suffering from chronic illnesses are emerging. Take diabetic patients, for example. If they do not have a device, diabetics have to report their blood glucose values to their doctor through manually recorded diaries. However, if they have a glucometer, a small sensor that measures continuously, this information is much more objective and accurate. Of course, all the information from the sensor represents a large amount of data that the doctor has to visualise when they examine the patient in the doctor’s office. This is where AI helps to identify which critical episodes the patient has had and makes recommendations so that they do not happen again. This reduces the time the doctor needs to process the information, time that can be spent on patient care[5].
Personalising treatments
The use of data has generally facilitated the application of AI algorithms to deliver personalised medicine and to provide personalised recommendations. But devices are not only present in patient care; medicine has long since shifted from the “disease” paradigm to the “health” paradigm, with professionals focusing on giving us recommendations to maintain quality of life, known as preventive medicine. In this context, wearables such as smartwatches help us to track our daily exercise, for example. There is also a range of mobile apps that track healthy habits and use AI to make suggestions based on our progress; however, it is important to consider those that are certified by the appropriate bodies.
AI has also made it possible for people to play an active role in their health process. Without AI, participatory medicine is limited to informing the patient about the disease they have; there are even educational games that help them understand what is the matter with them. But AI allows us to go one step further: one example is the development of robots that educate young children with diabetes[6].
With the TDApp tool, patients suffering from ADHD (attention deficit hyperactivity disorder) or their caregivers can express their preferences regarding the adverse effects they wish to avoid. Based on this information and the person’s clinical data, the TDApp application proposes a list of possible treatments, according to the most up-to-date medical evidence. If an adolescent patient, for example, does not wish to gain weight as a result of treatment, the system can suggest alternative medication. The psychiatrist makes the final decision, but, among drugs with a similar efficacy, they will be likely to choose one that meets the patient’s preferences, with the aim of ensuring the patient follows the treatment prescribed.
One of the fields in which AI is revolutionising medicine and healthcare the most is prediction (diagnosis). In particular, considerable progress has been made in medical imaging systems using deep learning methods to identify, for example, potential tumours. Recently, AI has shown that it can more accurately identify tumours than human experts can[7].
The 4Ps of medicine
AI is therefore embedded in the 4Ps of medicine: predictive, preventive, personalised and participative aspects[8]. There are many applications available, in all fields. According to the Catalan Observatory for AI in Health[9], 47.68% of the algorithms developed and registered are aimed at hospital care, 23.24% at primary care, and, to a much lesser extent, 8.61% at mental illnesses, and 7.28% in the social and healthcare field. In fact, one of the current challenges in medicine is mental health, and here AI can provide new tools related to the identification of emotional state from psychophysiological data collected by sensors (for example, measuring stress through cardiovascular data and skin sweating), which may be the precursor to more serious neurological diseases such as Alzheimer’s.
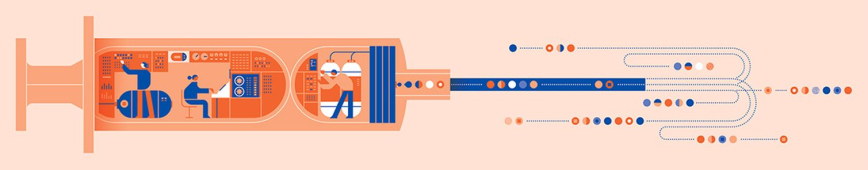 Illustration © Romualdo Faura
Illustration © Romualdo FauraIt is worth noting that only 17% of the algorithms are aimed at improving management, while 60.53% are dedicated to clinical practice and surgery. In the latter area, the important role of robotics is noteworthy. Robots such as Da Vinci or Bitrack[10] are supported by medical imaging systems that show the physician the most relevant information in each case. A complex surgery such as transcatheter aortic valve implantation (TAVI) would be difficult to understand today without the help of AI systems that provide support to clinicians at all times[11].
All these systems are also propelled by a reality: we have a very ageing population. Medicine must provide solutions for people who reach an advanced age with chronic diseases (such as respiratory diseases or hypertension), with comorbidities (suffering from more than one disease) and with limited healthcare resources to care for them. However, due to advances in medicine, there are many people who reach old age with a state of health that allows them to live autonomously at home. In this context, smart homes are emerging, equipped with sensors that allow a person’s life to be monitored and can detect if the person falls or is unable to get up[12].
Robotics is also accompanying these elderly people by providing them with carers to look after them in the realm of routine tasks and allowing them to share leisure time with their family members, who, thanks to this assistance, will not be worn out. The film Robot and Frank, which illustrates this future that lies ahead of us, is a case in point.
The opportunities for caring for the elderly are highly inventive. For example, the company Sound Intelligence has developed software to monitor noises in a nursing home: if the observed sequence corresponds to normal behaviour (such as a bed movement, followed by the noise of a door opening, water falling, a door closing and another bed movement), the system does not disturb the potential caregiver; but if the sequence of noises is abnormal (a bed movement and a loud bang), an alarm is set off[13]. And the system has to work on a stormy day!
In conclusion, we can say that one of the drivers of AI in medicine and healthcare is the availability of data. However, there are major challenges. Firstly, in terms of data quality, the occurrence of bias and privacy. Generative AI – ChatGPT being one of the most prominent examples – can open doors to new drugs and ultimately generate new hypotheses and treatments, but it poses huge challenges regarding the body of data on which the results are generated, which can lead to significant biases[14].
Secondly, with regard to the transparency of the systems: the solutions provided by AI algorithms must be comprehensible to merit the trust of professionals. There is still a road ahead of us that needs to be tackled in terms of legislation, with the corresponding regulations for use.
The prime example of the potential of AI is the case published in 2022, which described a paraplegic being able to walk again thanks to implants.
But let’s concentrate on the opportunities. And the prime example is the one published in 2022 on research by the Swiss Federal Institute of Technology in Lausanne, Switzerland, which shows how a paraplegic person, confined to a wheelchair, can walk again thanks to AI-controlled implants[15].
[1]Shortliffe, E. H. “A rule-based computer program for advising physicians regarding antimicrobial therapy selection”. ACM National Conference. 1974. http://ow.ly/KUFh50OnBSz
[2]Rajpurkar, P., Chen, E., Banerjee, O. i Topol, E. J. “AI in health and medicine”. Nature Medicine. 2022. http://ow.ly/Tgbi50OnBTU
[3]Ferruz, N., i Höcker, B. “Controllable protein design with language models”. Nature Machine Intelligence, 4, 521-532. 2022. http://ow.ly/XXuL50OnBUy
[4]Goh, K. H., Wang, L., Yeow, A. Y. K., Poh, H., Li, K., Yeow, J. J. L. i Tan, G. Y. H. “Artificial intelligence in sepsis early prediction and diagnosis using unstructured data in healthcare”. Nature Communications 2021, 12 (1), 1-10. 2021. http://ow.ly/oURa50OnBVn
[5]Torrent-Fontbona, F. i López, B. “Personalized Adaptive CBR Bolus Recommender System for Type 1 Diabetes”. IEEE Journal of Biomedical and Health Informatics, 23(1), 387-394. 2019. http://ow.ly/ALPK50OnBXb
[6]Sánchez, E. “Un robot que ayuda a los niños con diabetes”. Euronews. 2017. http://ow.ly/iaOv50OqOVy
[7]“AI ‘outperforms’ doctors diagnosing breast cancer”. BBC News. 2020. http://ow.ly/KjAg50OnBZ9
[8]Flores, M., Glusman, G., Brogaard, K., Price, N. D. i Hood, L. “P4 medicine: how systems medicine will transform the healthcare sector and society”. Personalized Medicine, 10(6), 565. 2013. http://ow.ly/Rrwx50OnC0f
[9] “Identificació d’algorismes d’IA”. Observatori IA en salut. http://ow.ly/gKUg50OnC1J
[10]RobSurgical. Bitrack System. https://www.robsurgical.com/es/
[11]El-Fakdi, A., Gamero, F., Meléndez, J., Auffret, V. i Haigron, P. “A framework for a workflow-based CBR for interventional Clinical Decision Support Systems and its application to TAVI”. Expert Systems with Applications. 2014. http://ow.ly/Vj0750OnC2R
[12] Zoë, C. “The future of elder care is here – and it’s artificial intelligence”. The Guardian. 2021. http://ow.ly/X5fN50OnC4r
[13]Audio analytics for professionals. https://www.soundintel.com/
[14]Zhavoronkov, A. “Caution with AI-generated content in biomedicine”. Nature Medicine. 2023. http://ow.ly/SKy050OqPa1
[15] Barraud, E. “New implant offers promise for the paralyzed”. EPFL, 2022. http://ow.ly/OEbe50OqPh7. Open in a new window
The newsletter
Subscribe to our newsletter to keep up to date with Barcelona Metròpolis' new developments